The term osteochondrosis itself comes from two words: osteo - bone and chondrue - cartilage. Simply put, it is the ossification of cartilage. Although this interpretation is fundamentally wrong. Some go even further in their delusions, and are convinced that osteochondrosis is the deposition of salts in the joints. In addition, it is the table salt that is supposed to be consumed in large quantities for food.
Pathogenesis
In fact, everything becomes a little different. And more difficult. And table salt, if it plays a role in the development of osteochondrosis, is very indirect. Osteochondrosis is based on the degeneration and degeneration of articular cartilage. This is not an independent disease, but a pathological process that can occur almost anywhere where there is cartilage connective tissue.
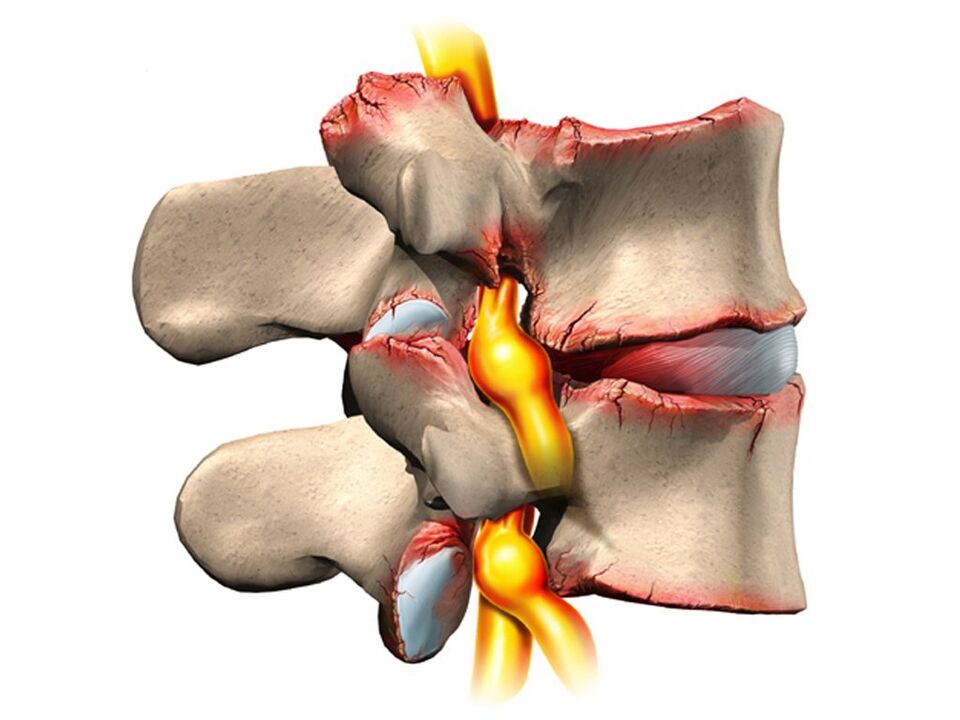
Also, osteochondrosis in the overwhelming case affects the spine. Because this? The fact is that between the vertebrae there is a kind of cushion - intervertebral (intervertebral) discs. The normal role of these discs is to protect and safeguard the vertebral bodies from premature wear due to mechanical stress. The disc consists of an inner fluid pulposus nucleus surrounded by a fibrous ring and an upper and lower end plate.
The disk is under tremendous mechanical stress, which leads to permanent damage to its structures at the cellular level. To humans, these processes are very intense - this is our payment for walking upright. In order to avoid the complete "deletion" of the disk, it must be constantly regenerated, that is, it must be rebuilt. It is the balance of damage-regeneration processes that determines the normal structure of the intervertebral disc. Another strange detail is that the supply of blood and nutrients to the intervertebral discs takes place not through blood vessels, which are overgrown in childhood, but diffused, from the bone tissue of the vertebral bodies. Again, pay for mobility in two extremes, not four.
Because of this, the intervertebral discs are easily injured anatomically and physiologically. Any negative process in the body leads to an imbalance in the damage-regeneration balance and to the development of dystrophy and degeneration in the discs. A structurally defective disc can no longer withstand the proper mechanical stress. Under excessive pressure from the overlying vertebrae, the discs move in different directions, usually sideways and backwards. This procedure is called a disc herniation.
The bone tissue of the vertebrae, which has lost its cartilaginous lining, also undergoes mechanical damage. Due to continuous trauma to the surface of the anterior limb of the vertebral bodies, abnormal bone growths are formed - osteophytes. Spondylosis develops. Due to degeneration and displacement of the disc, the intervertebral spaces are reduced, the spinal canal narrows and the roots of the spinal nerves in the so-called spinal cord holes are violated.
Causes
The causes or etiological factors of osteochondrosis are varied. They can be both local, ie due to the pathology of the spine itself, and general disorders at the organism level. Any pathology that leads to a violation of the structure of the spine or metabolic disorders can be considered as the cause of osteochondrosis. In this regard, there are:
- Changes in the shape of the spine (scoliosis, abnormal lordosis or kyphosis).
- Other defects of the musculoskeletal system are flat feet, narrow shoulder girdle, abnormalities in the structure of the pelvis.
- Spinal cord injury.
- Weak immunity.
- Metabolic disorders - osteoporosis, obesity, diabetes, thyroid disease.
- Diseases of the cardiovascular system - atherosclerosis, hypertension.
- Digestive disorders that lead to insufficient absorption of nutrients from the gastrointestinal tract.
- Heredity.
It should be noted that the above pathological conditions do not necessarily lead to osteochondrosis. This requires constant exposure to certain predisposing factors - hypothermia, malnutrition, sedentary lifestyle or, conversely, excessive physical exercise.
Symptoms
Osteochondrosis itself is an asymptomatic process. And, at the same time, the signs of intervertebral disc degeneration are varied. How come? The fact is that the clinical manifestations of osteochondrosis are based on its complications - disc herniation, spondylosis, sciatica, narrowing of the spinal canal.
In addition, the clinic is highly variable depending on the predominant localization of the procedure in the cervical, thoracic or lumbar spine. The last part is most often affected, as it is the lower back that undertakes the maximum physical activity. Signs of osteochondrosis of the lumbar region:
- Pain (low back pain, back pain, sciatica).
- Restriction of movement in the lower back and lower extremities (intermittent lameness).
- Here, sensory disturbances of the paraesthesia type - numbness, burning, crawling.
- Pathological tension of the lumbar muscles.
- In the absence of treatment, disorders of the pelvic organs.
Cervical osteochondrosis is somewhat less common than lumbar osteochondrosis. However, this pathology is also quite common. In addition to the typical signs of pain (neck pain), decreased sensitivity and movements in the upper extremities, cervical osteochondrosis due to reduced blood supply to the brain has its own characteristics. These characteristics are manifested:
- Insomnia.
- Headache, dizziness.
- Periodic nausea.
- General weakness, rapid fatigue.
- Fluctuations in blood pressure.
- Occasional toothache.
- Behavioral reactions in the form of tearing, irritability.
The thoracic region with osteochondrosis is relatively rare. Patients in this case are people who are forced to sit in a fixed uncomfortable position due to profession - students, pupils, programmers, office workers. The symptoms of osteochondrosis in this case will be the following:
- Chest pain and hallucinations.
- Shortness of breath.
- Feeling of heartbeat.
- Restriction of movement in the thoracic spine.
Diagnostics
From all this it is clear that osteochondrosis is a chameleon disease. Due to the similarity of the signs, it is easy to confuse it with cerebrovascular accident, hypertension, myocardial infarction, angina, neurotic disorders. Therefore, in order to make the correct diagnosis, a complete complex diagnosis is necessary for the correct identification of the symptoms and the treatment of osteochondrosis.
This diagnosis, in addition to the traditional challenge and clarification of patients' complaints, should include medical examination and special research methods. These methods include x-ray of the spine, ultrasound of internal organs. Recently, computed tomography and MRI scans have been used successfully to diagnose osteochondrosis.
Treatment
Therapeutic tactics for osteochondrosis include the use of:
- Medicines.
- Massage.
- Physiotherapy procedures.
- Physiotherapy (ascotherapy).
- Manual therapy.
- Acupuncture.
Medication for osteochondrosis is mainly aimed at relieving pain and eliminating inflammatory processes in the nerve roots. In various combinations, these drugs are widely used in the form of ointments, injections, tablets to treat osteochondrosis. We must not forget that these drugs have a negative effect on the liver, stomach and intestines. With this, they can worsen the metabolic disorders in osteochondrosis. They relieve the pain of exclusion well with local anesthetics. It is true that the effect of these funds is short-lived and in no way affects the course of osteochondrosis as a whole.
It is possible to improve metabolic processes locally and physically with the help of drugs such as chondroprotectants, immunostimulants and vitamins with minerals. Chondroprotectants are used in tablets, ointments and ampoules. Among the enhancers, vitamins C, group B, are used in combination with minerals. In this regard, calcium preparations are more preferred. Indeed, contrary to some misconceptions, the basis of osteochondrosis is not an excess, but simply a lack of calcium.
After the successful relief of the flare-up, physiotherapy, massage and exercise therapy procedures appear. As natural procedures, calcium electrophoresis, hydrocortisone phonophoresis, ampullae, paraffin therapy are used. All of these measures are aimed at eliminating pain and inflammation in the nerve roots, ligaments and muscles. The massage for osteochondrosis is performed according to the generally accepted method. The massage zone is selected depending on the location of the osteochondrosis. Widening of the range of motion is achieved with the help of exercise therapy. In the beginning, in the phase of exacerbation, there are practically no dynamic loads. The patient is constantly in the optimal position. At this time, it is desirable to wear immobilizers - lumbar corset, neck collar Shants. As the exacerbation subsides, the volume and duration of movements during exercise therapy increase.
Recently, in the treatment of osteochondrosis, non-traditional methods of treatment have been received - acupuncture, manual therapy, osteopathy. Acupuncture is an effect on special biologically active points located along the spine, ears, hands and feet. With manual therapy, the normal position of the vertebrae and intervertebral discs is restored by the manual action of a specialist's hands. In the course of osteopathy, the structural integrity of the musculoskeletal system is ensured by using specific techniques. In the absence of the effect of conservative measures for the treatment of osteochondrosis, persistent pain, complications, surgery is indicated. The abnormally displaced disc is removed. At present, microdiscectomy is performed for this purpose - endoscopic removal of a displaced disc.















































